Introduction:
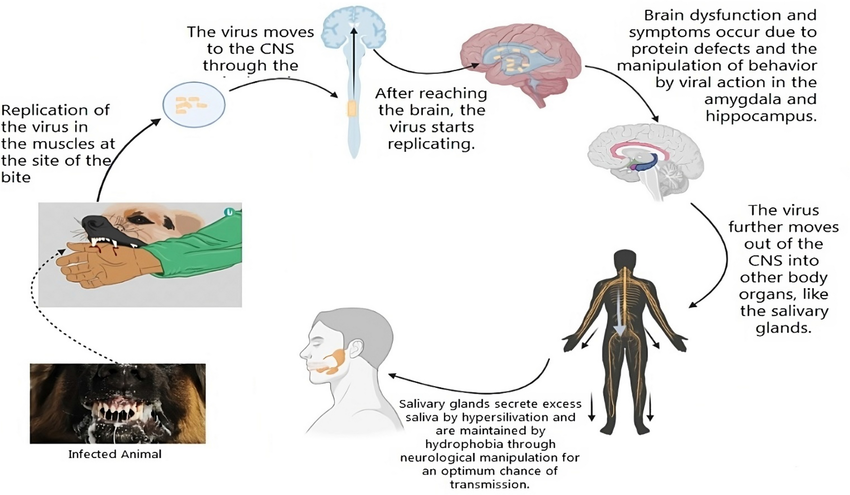
Rabies is an acute viral disease that causes fatal encephalomyelitis in virtually all warm-blooded animals including man. The virus is found in wild and some domestic animals and is transmitted to other animals and humans through their saliva (following bites, scratches, licks on broken skin and mucous membrane). In India, dogs are responsible for about 95% human rabies, followed by cats (2%), jackals, mongoose and others (1%). Therefore, the disease is mainly transmitted by the bite of a rabid dog.
Fortunately, the development of Rabies can be prevented to a large extent if animal bites are managed appropriately and in time. In this regard, the post-exposure treatment of animal bite cases is of prime importance.
When to give a rabies vaccine?
- Dog/cat bite (even if vaccinated)
- Exposure to wild animals (considered as category III as described below)
- Exposure to wild rodents
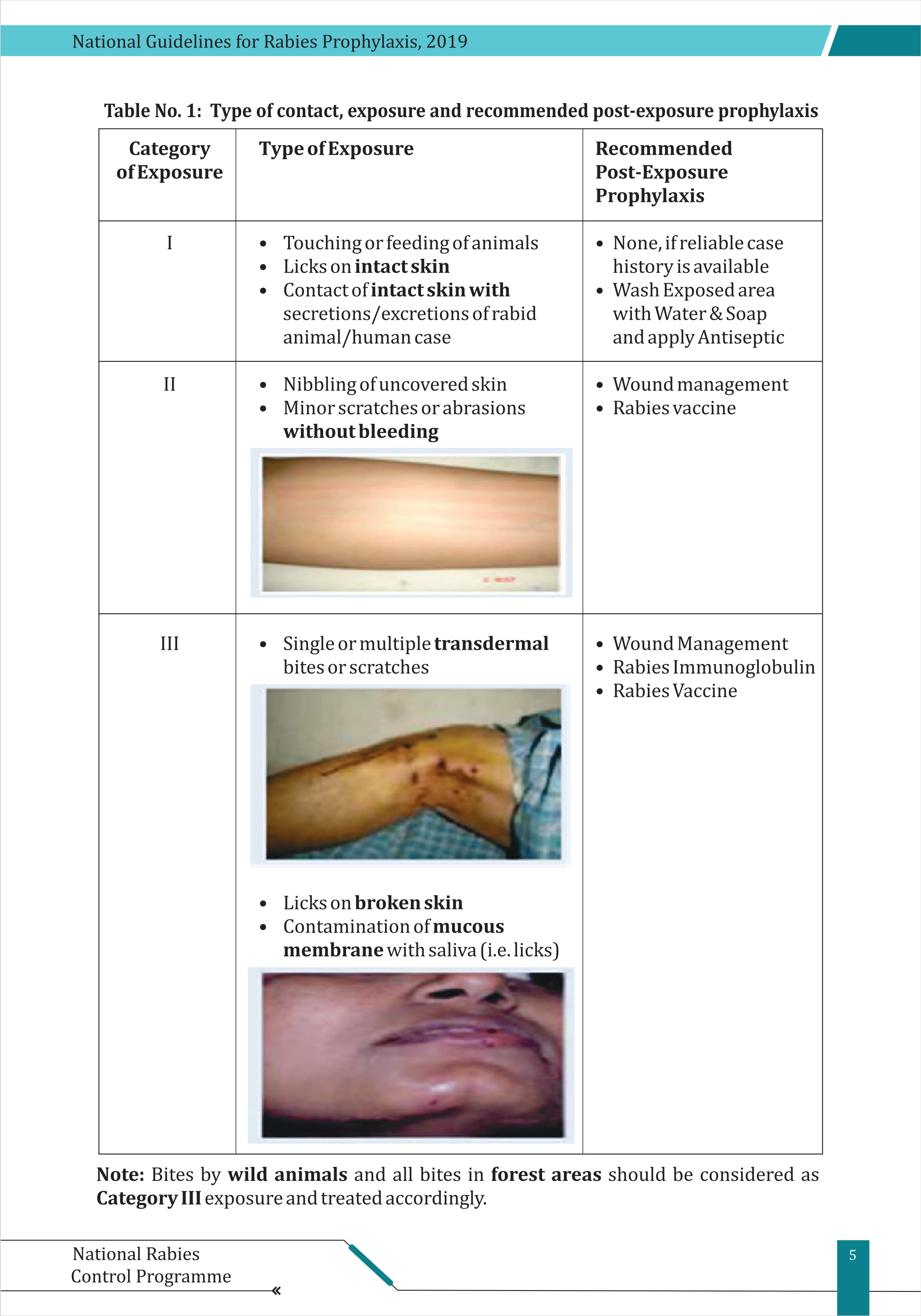
What are the types of exposure?
When and how to give the anti-rabies vaccine (ARV)?
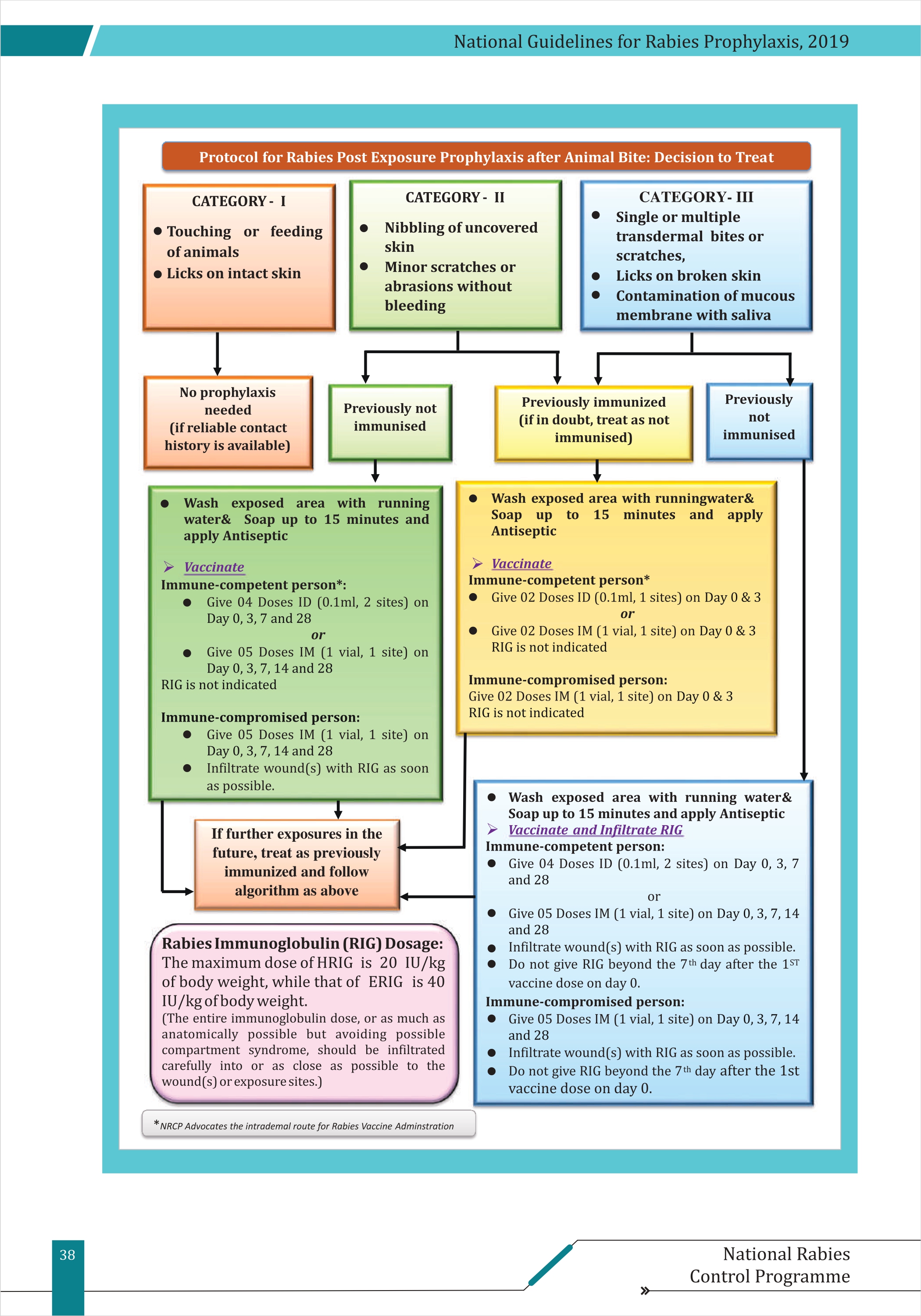
When to give ARV: category II, category III (generally also given in category I due to concerns about the reliability of the case history)
How to give ARV:
- ID (0.1 cc + 0.1 cc) at both the deltoid muscles or
- IM (0.5 cc). Both are equally effective, but ID is less effective in immunocompromised patients, so IM is preferred where patient load is high.
Regimens:
- ID (0, 3, 7, 28)
- IM (0, 3, 7, 14, 28)
Preferred sites:
- Adults (deltoid)
- Infants (anterolateral part of thigh)
Some considerations:
- Switching from one regimen to another or from one vaccine to another type is not recommended, but, if required, there is no need to restart the regimen; just continue with the newer regimen.
- Adequate titre is 0.5 IU/ml, which is achieved after 14 days of the first vaccine dose.
When to give immunoglobulins?
- If category III wounds: all new patients
- Category II & category III wounds in immunocompromised patients
Types of RIG (Rabies Immunoglobulin):
- ERIG (equine) - 40 IU/kg
- HRIG (human) - 20 IU/kg (because it has a longer half-life)
Some considerations while giving RIG:
- Not recommended beyond 7 days after the first vaccine dose (whether the rest of the doses were taken or not).
- The entire RIG is to be administered into the wound or as near as possible to the wound using a syringe and needle (as much as anatomically possible; avoid compartment syndrome). Remaining RIg can be given IM (but provides very little or no protection).
- Never administer RIg using the same syringe or at the same site of vaccine administration.
- Never give RIg intravenously.
- A testing dose (0.2 cc) is given but is not conclusive of an adverse reaction. Even if the test is negative, it can give rise to anaphylaxis (though very rare).
- Observe the patient for 15-20 minutes after giving Ig.
What to do in case of re-exposure?
- If the patient received a complete regimen (documented)—two doses (0, 3), no RIG. Else, treat it as a new case.
- If re-exposure takes place while the regimen is not complete yet, there is no need to restart the regimen. Just complete the remaining doses.
Are there any contraindications for ARV?
None (Can be given to infants, old, pregnant, or lactating women)
Patients taking chloroquine for malaria may have reduced response to intradermal inj. They should receive intramuscular injection.
Wound care:
- Clean the wound with soap and water.
- Wash the wound with soap or antiseptic.
- Suturing, if needed, should be delayed for several hours.
- Inj TT (0.5 cc IM) is also given along with the first dose of the vaccine.
- Give suitable antibiotics and painkillers as required.
Summary:
References:
https://ncdc.mohfw.gov.in/wp-content/uploads/2024/02/Guidelines-for-Rabies-Prophylaxis.pdf